Post Time: 2025-07-26
High blood glucose, also known as hyperglycemia, occurs when there's too much sugar (glucose) circulating in the blood. This is a hallmark of diabetes but can also occur in non-diabetic individuals under specific circumstances. It’s crucial to recognize the early signs of high blood glucose to prevent serious health complications.
Why does it happen? Glucose is your body's primary source of energy, derived from the food you eat. Insulin, a hormone produced by the pancreas, helps glucose move from the bloodstream into your cells for energy. In cases of diabetes or insulin resistance, this process doesn't work efficiently, resulting in excess glucose in the blood.
Common Symptoms of Hyperglycemia:
Recognizing these early symptoms is key to managing blood sugar levels effectively. Ignoring these signs can lead to both immediate discomfort and serious long-term health issues, particularly affecting nerve health.
| Symptom | Description | Why it Occurs |
|---|---|---|
| Frequent Urination | Needing to pee more often than usual, especially at night | The kidneys are trying to get rid of the excess glucose by excreting it through urine. |
| Excessive Thirst | Feeling unusually thirsty despite drinking water. | High glucose draws water out of your cells into the bloodstream, causing dehydration, and thus the sensation of thirst. |
| Fatigue | Feeling tired and lethargic despite sufficient rest. | Cells aren't getting sufficient glucose for energy, leading to a feeling of exhaustion. |
| Blurred Vision | Difficulty in seeing clearly. | High glucose levels can affect the fluid balance in the eyes, leading to temporary blurring. |
| Headaches | Experiencing frequent or severe headaches. | Fluctuating blood sugar levels can sometimes trigger headaches and migraines. |
A Quick Summary: The symptoms of high blood glucose result from the body’s attempt to manage the excess glucose. Recognizing these symptoms is the first step in seeking timely medical help and preventing severe consequences, including nerve damage.
The Link Between Long-Term High Blood Glucose and Nerve Damage
The insidious danger of chronic hyperglycemia lies in its ability to cause gradual, yet significant, damage to various organ systems, with nerve health being particularly vulnerable. Prolonged exposure to elevated blood glucose levels can lead to a condition known as diabetic neuropathy.
How Does High Blood Glucose Damage Nerves?
Here’s a more in-depth look into the mechanisms involved:
- Microvascular Damage: Persistent hyperglycemia damages the small blood vessels (microvasculature) that supply the nerves with oxygen and nutrients. This reduced blood flow deprives the nerves of essential resources, leading to nerve dysfunction and damage. This damage affects sensory and autonomic nerves.
- Direct Glucose Toxicity: Excess glucose can be directly toxic to nerve cells, particularly the myelin sheath (protective coating around nerve fibers). This sheath allows electrical signals to travel efficiently through nerve cells. Damage to the myelin can cause reduced nerve signal transmission.
- Formation of Advanced Glycation End-products (AGEs): Glucose binds to proteins and fats, forming harmful compounds called AGEs. These AGEs accumulate in nerve tissue and blood vessel walls, causing oxidative stress, inflammation, and further damage to nerve cells.
Types of Diabetic Neuropathy:
- Peripheral Neuropathy: This is the most common type, affecting the nerves in the feet and legs, and hands. It manifests through tingling, numbness, pain, or a burning sensation. In severe cases, it can lead to ulcers, infections, and even amputation.
- Autonomic Neuropathy: This affects nerves that control involuntary functions, such as heart rate, blood pressure, digestion, and bladder function. Symptoms vary but can include heart rhythm problems, digestive issues, and sexual dysfunction.
-
Proximal Neuropathy: This causes pain in the thighs, hips, or buttocks, often accompanied by muscle weakness. It may cause difficulty with movements such as standing from a sitting position.
Here's a detailed overview of how nerve damage can vary in diabetic individuals:
Type of Neuropathy Affected Area Common Symptoms Peripheral Feet, legs, hands, arms Tingling, numbness, burning pain, sensitivity to touch Autonomic Organs (heart, stomach, bladder) Digestive issues, bladder problems, abnormal sweating, dizziness Proximal Thighs, hips, buttocks Pain, muscle weakness, difficulty rising from seated position
Real-World Data:
According to a study by the American Diabetes Association, approximately 50% of people with diabetes develop some form of neuropathy. The risk of neuropathy increases with the duration and severity of high blood sugar levels. Early detection and intervention are critical to slowing down or preventing this nerve damage progression.
In essence: High blood sugar is not just about short-term discomfort. Chronically elevated levels can lead to microvascular issues, direct cellular damage, and the formation of harmful compounds, severely impacting nerve health and leading to long-term complications such as diabetic neuropathy.
Practical Strategies for Preventing and Managing High Blood Glucose and Protecting Nerve Health
Preventing or managing high blood glucose is paramount for maintaining nerve health. It involves several proactive strategies that combine lifestyle adjustments with medical care. Here’s how you can take control:
1. Regular Blood Glucose Monitoring:
- Home Monitoring: Use a glucose meter to monitor your blood glucose levels several times a day, particularly before meals, 1-2 hours after meals, and before bedtime, according to your healthcare provider’s advice.
- Continuous Glucose Monitoring (CGM): Consider using a CGM device if recommended by your doctor. CGM provides real-time glucose readings, offering more comprehensive insights into blood sugar trends.
2. Dietary Management:
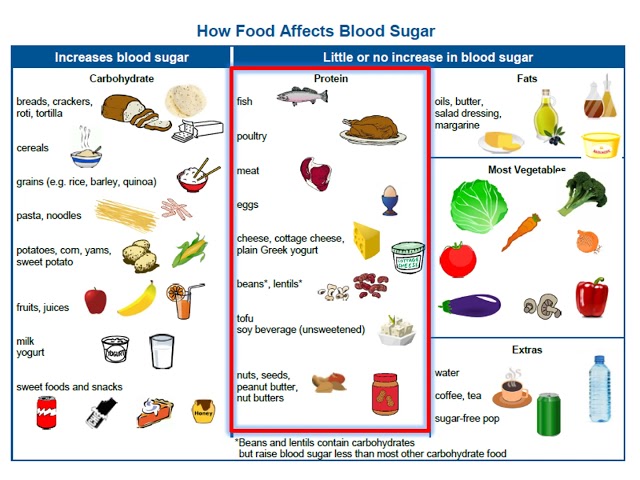
- Balanced Meals: Emphasize a balanced diet rich in fiber, lean proteins, and healthy fats. Limit refined carbohydrates and sugary drinks.
- Portion Control: Manage your intake through controlled portion sizes. Work with a dietitian to create a meal plan tailored to your individual needs.
- Carbohydrate Awareness: Learn about carbohydrate counting to manage the impact of food on your blood glucose. Not all carbs are created equal, so prioritize complex, high-fiber options.
- Glycemic Index and Glycemic Load: Be mindful of the Glycemic Index (GI) and Glycemic Load (GL) of foods as higher GI and GL can result in spikes in blood sugar.
3. Regular Physical Activity:
- Aerobic Exercise: Engage in at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, jogging, or swimming.
- Strength Training: Incorporate strength training exercises at least two to three times a week. This can help improve insulin sensitivity and muscle function.
- Consistency is Key: Consistency in your exercise routine is more important than intensity, as regular exercise helps improve insulin sensitivity, leading to better blood sugar control.
4. Medication Adherence:
- Follow Doctor's Instructions: If your doctor prescribes medication, take it as directed.
- Regular Check-ups: Schedule regular appointments with your healthcare team to monitor your condition and adjust your treatment plan as necessary.
- Open Communication: Communicate with your medical team about any issues you encounter with medications or your blood sugar levels.
5. Stress Management:
- Relaxation Techniques: Employ relaxation techniques like yoga, deep breathing, or meditation to reduce stress levels, which can impact blood glucose.
- Adequate Sleep: Ensure you are getting adequate sleep, as lack of sleep can negatively affect blood sugar levels.
6. Foot Care:
- Daily Inspection: Routinely inspect your feet for any cuts, blisters, or swelling due to the higher risk of neuropathy that can impair sensation and lead to injury that could go unnoticed.
- Appropriate Footwear: Wear comfortable, well-fitted shoes to prevent sores and ulcers from developing.
7. Education and Support:
- Diabetes Education Programs: Participate in a diabetes education program to learn more about your condition and effective management strategies.
- Support Groups: Join a diabetes support group for emotional support, sharing experiences, and gaining knowledge from others living with diabetes.
Example of a Practical Approach:
- Scenario: An individual diagnosed with Type 2 diabetes struggles with post-meal spikes in blood sugar.
- Solution: Following their dietitian’s guidance, the person starts implementing strategies like:
- Adding a portion of high-fiber vegetables and protein to each meal.
- Walking for 20 minutes post meal to improve glucose use.
- Learning carbohydrate counting to maintain glucose within their target range.
Summary of Steps: Through diligent monitoring, targeted dietary changes, regular exercise, medication adherence, stress management, and a strong commitment to self-care, people can minimize the effects of high blood glucose and protect their nerve health, reducing their risks of complications like diabetic neuropathy.
By implementing these comprehensive strategies, individuals can manage blood glucose effectively and significantly reduce the long-term impacts on nerve health and improve overall wellbeing.
An overview of how food affects your blood blood sugar 3 hours after eating reddit sugar. a1c 6.8 average blood sugar what to do to lower your blood sugar